Breaking News: Cutting-Edge Innovations as Gough Surgical, PLLC Supercharges Advanced Robotic Orthopedic Surgery – Only on Planet TV Studios's Documentary Series New Frontiers!
Planet TV Studios displays a documentary regarding Dr. Brandon Gough's Cutting-edge Surgical Developments within "New Frontiers" – Airing Early 2024 across National Broadcast plus Video On-Demand.
BOCA RATON, FL, UNITED STATES, March 2, 2024 /ReportWire.org -- Planet TV Studios with pride showcases its cutting-edge documentary project, "New Frontiers," showcasing the innovative milestones by Gough Surgical, PLLC. This series delves deeply into the revolutionary progressions led by Dr. Brandon Gough, M.D., a foremost specialist in orthopedics specializing in minimally invasive methods as well as advanced robotic joint replacement for hips and knees.
"New Frontiers" constitutes a spellbinding adventure expertly crafted in order to exhibit trailblazing organizations directing the next generation of healthcare worldwide. Tune in to watch the documentary segments premiering in Q2 2024 across the national airwaves, Bloomberg TV, and accessible on-demand through platforms such as the Amazon digital hub, Google Play Video, Roku, and other services.
Planet TV Studios is gratified to feature Gina Grad rejoining as the anchor. Gina is a renowned literary figure, podcast emcee, and on-air personality located in Los Angeles, California. She previously served as sharing the role of co-host and news anchor on the Adam Carolla Show, a record-breaking podcast in terms of downloads. Gina has fulfilled anchoring duties on KFI 640 AM while also hosting the mornings at 100.3 FM. She is the current host of "The Bryan and Gina Show, The Official Podcast of LA Magazine." Besides her on-air career, she created "My Extra Mom," a storybook developed to aid young readers and stepparents with the nuances of modern blended families.
Dr. Brandon Gough, M.D., stands as an exceptionally respected orthopedic specialist, board certified and renowned for his expertise in arthroplasty of the hip and knee across Phoenix, Arizona. Adopting breakthrough robotic technology in tandem with minimally invasive surgical techniques with muscle preservation, Dr. Gough strives to promote speedy returns to dynamic lives for his patients after surgery. His focus on maintaining soft tissue integrity fosters speedy recuperation, curtails hospital stays and, in specific situations, enables total joint replacement in an outpatient setting. He is celebrated as an international pioneer in the Direct Superior Approach and muscle-sparing robotic-assisted methods.
In Dr. Gough’s practice, education is key, serving as the bedrock for premium patient care via ongoing learning in orthopedic advancements. Upon finishing his undergraduate education at Spring Hill College in the city of Mobile, Alabama, he obtained his medical degree from Creighton University School of Medicine at Omaha, Nebraska. He further polished his skills by completing residency and internship in General Orthopedics at the University of Kansas, School of Medicine from Wichita, KS, where he earned recognition as the Resident Teacher of the Year. He continued to specialize with a fellowship in Lower Extremity Adult Reconstruction at the Arizona Institute of Bone and Joint Disorders.
Being board-certified by the American Board of Orthopedic Surgeons and actively involved with organizations like the American Academy of Orthopedic Surgeons (AAOS), Dr. Gough's resolution towards excellence surpasses his routine practice. He simultaneously leads the Orthopedic Surgery Interest Group as Vice President and maintains active memberships with both the AMA and ACP. His practice is based at the prestigious Orthopedic Institute of the West, a center he assisted in founding, and he maintains surgical privileges at Scottsdale Abrazo Hospital, Liberty Hospital, as well as select surgery centers throughout the Phoenix/Scottsdale, AZ region. Embodying his dedication to surgical progress, he leads the charge in establishing a center of excellence for robotic hip and knee replacements and generously shares his knowledge with surgeons globally.
Alongside his medical practice, Dr. Gough persistently devotes himself to community engagement, offering volunteer services to organizations such as the Magis Clinic, Madonna School, Habitat for Humanity, and Sienna St. Francis Clinic.
Notably, Dr. Gough serves as a consultant and educator for Zimmer Biomet, further solidifying his commitment to advancing orthopedic care and surgical techniques.
An Introduction to Planet TV Studios: Planet TV Studios crafts state-of-the-art, real-world television series that provide thoughtful updates on significant business, medical, and ethical issues.
For more information about Gough Surgical, PLLC, please visit https://goughmd.com.
For additional series insights, visit https://planettvstudios.com and https://planettvstudios.com/backstage/ or reach out to Christian Alain at 888-210-4292 x100 or email christian@planettvstudios.com.
Gough Surgical Adult Hip & Knee: Guiding Upcoming Era in Musculoskeletal Treatment
Throughout the domain of joint and bone operations, precision, experience, and innovation unite at Gough Surgical Adult Hip & Knee, an esteemed practice specifically catering to adult lower joint replacements.
Led by the expertise of Dr. James Gough, this dedicated facility has secured honors for changing lives by regaining motion, mitigating suffering, and remarkably uplifting life standards for a multitude of patients.
Defining New Criteria in Orthopedic Surgery
Skeletal procedures, concerning predominantly hip and knee regions, stand as among the most frequently performed treatments conducted internationally.
Still, the success statistics and patient experience ratings differ considerably attributable to technical ability, hospital standards, and the doctor's approach.
Gough Surgical is set apart by committing exclusively to adult joint replacement procedures, permitting deep specialization not common in broader practices.
Dr. James Gough, acknowledged for his precise surgical methods and patient-oriented service, has devoted his vocation to excelling in these challenging interventions.
His clinic, Gough Surgical Adult Hip & Knee, well-located to serve a diverse patient base, has become emblematic of high-quality results, quick recoveries, and high patient satisfaction metrics.
Excellence Founded on Expertise
Why dedicate practice solely to adult hip and knee replacements?
Based on Dr. Gough's insights, focusing on a niche yields unrivaled skill.
"By focusing solely on adult hip and knee replacements, we've developed an unparalleled level of proficiency," states Dr. Gough.
This specific mastery translates into reduced issues, minimized surgical dangers, and improved patient experiences.
Innovative Surgical Methods and Equipment
Gough Surgical Adult Hip & Knee steadily employs advanced technological solutions to boost procedural precision and patient outcomes.
One of the clinic's standout features involves using cutting-edge robotic-assisted surgical equipment.
These progressive tools allow exceptional precision, resulting in accurate prosthetic positioning designed for each patient's specific anatomy.
"Robotic assistance doesn't replace the surgeon's expertise—it enhances it," asserts Dr. Gough.
Patient-Centric Care: Surpassing Basic Procedures
At Gough Surgical, care for patients goes well beyond the operating room.
From initial assessment through extensive post-surgery reviews, personalized care is provided continuously to every patient.
This all-encompassing approach facilitates physical recovery and nurtures psychological reassurance and self-assurance throughout the healing journey.
Dr. Gough asserts, "Comprehending the unique necessities, apprehensions, and targets of each patient is key." Personalized care significantly impacts recovery rates and overall patient satisfaction.
Comprehensive Pre- and Post-Operative Support
Gough Surgical’s promise of integrated support shows itself via its in-depth preoperative protocols and comprehensive postoperative check-ups.
Customized pre-surgical classes, in-depth patient seminars, and face-to-face consultations prepare patients physically and mentally, mitigating worry and nurturing informed selections.
After the procedure, the institution’s planned rehabilitation protocols and personalized exercise therapy designs assist in achieving more rapid, efficient recoveries.
Patients benefit from the precise advice, routine monitoring of their progress, and effortless access to professional insights, profoundly enriching their post-operative recovery.
State-of-the-Art Answers to Complex Problems
Gough Surgical Adult Hip & Knee excels in managing complicated cases that other facilities might find challenging.
Spanning from multifaceted joint reoperations to managing critical arthritis conditions, this center provides novel treatments using refined operative methods, less invasive procedures, and bespoke implant options.
These these tailored treatments typically produce rapid recovery, decreased postoperative aches, and rejuvenated movement, allowing individuals to return to vibrant, pain-free living with speed.
An Enduring Record of Patient Approval
The reviews from patients underscore the transformative power of its care.
Individuals consistently note re-established independence, noteworthy pain mitigation, and a heightened standard of living post-procedure.
"Walking without pain was something I never imagined possible again," states Mary Thompson, who experienced a total knee replacement at Gough Surgical.
"Dr. Gough and his team didn't just restore my knee—they gave me my life back," declares Mary Thompson subsequently.
Advancements in Research and Education
Beyond treatment excellence, Gough Surgical Adult Hip & Knee actively fuels advancements in orthopedic care with continuous research and training.
Dr. Gough regularly participates in clinical trials, contributing valuable data that advances orthopedic knowledge and patient care practices.
Additionally, the clinic holds regular educational events and practical workshops, nurturing collaborative learning among professionals and continuously advancing industry criteria.
A Cutting-Edge Approach to Orthopedic Treatment
As orthopedic practices continue to develop, Gough Surgical remains a trendsetter in orthopedic care, constantly embracing the latest technologies and methods.
The practice’s commitment to perpetual advancement guarantees that patients benefit from the latest, most efficient treatment modalities.
"{Our goal is to redefine what's possible in orthopedic surgery continually," explains Dr. Gough.
"Innovation and patient care must evolve hand-in-hand," continues Dr. Gough.
In Conclusion: Shaping the Future of Hip & Knee Treatment
Gough Surgical Adult Hip & Knee serves as a symbol of superior orthopedic treatment by combining state-of-the-art surgical methods, focused expertise, and heartfelt patient interaction.
By unremittingly driving innovation beyond norms, Dr. James Gough and his devoted professionals not only revitalize joint performance—they significantly uplift patient lifestyles.
In the path to a pain-free existence and renewed life force, Gough Surgical Adult Hip & Knee does not only change orthopedic paradigms—it lays down new foundations for the future of healthcare.
Minimally-injurious and Muscle-Sparing Surgical Methods: Reshaping Current Medical Practice
During the past several decades, surgical innovation has redefined patient care, promising lessened trauma, faster recovery, and improved outcomes.
Among these advancements, minimally invasive and fiber-preserving methods have emerged as transformative techniques.
These strategies have not only redefined the operating theater, but also revolutionized the clinical experience.
This discussion delves into the evolution, tactics, benefits, challenges, and prospective directions of micro-invasive and muscle-sparing surgery, drawing on expert insights, clinical studies, and real-world applications.
A New Era in Surgery: The Rise of Minimally Invasive Approaches
The modern operating room is a far cry from the large incisions and extended hospital stays that characterized surgery a century ago.
Surgeons today are consistently using approaches that minimize disruption of tissues and retain anatomical naturalness.
Fundamental to these breakthroughs are found micro-invasive and tissue-sparing approaches.
This approach, micro-invasive surgery, implies techniques that use small incisions, specialized instruments, and high-definition imaging to access and treat internal conditions with minimal disruption to surrounding tissues.
In contrast, muscle-guarding surgery underscores the conservation of muscle tissue integrity during interventions that traditionally involved extensive dissection.
Each approach forms part of a broad strategy to lessen patient morbidity, distress, and recovery intervals.
Retrospective Insights: Evolving from Open Surgery to Tissue Preservation
Surgical operations were long steered by necessity and prevailing technological capabilities.
In the period preceding modern imaging and advanced instrumentation, surgeons often had no alternative but to perform large, open incisions to gain adequate visibility and access to the operative site.
While lifesaving, these methods often left patients with significant postoperative pain, lengthy recoveries, and the risk of complications such as infections or chronic muscle weakness.
The change started with the emergence of laparoscopic surgery in the late 20th century—a minimally disruptive technique that provided internal Check This Out visualization using a diminutive camera inserted through minor incisions.
With technological progress, surgeons increasingly recognized that safeguarding muscle integrity in procedures could yield superior advantages.
techniques for muscle preservation, first pioneered in orthopedics and cardiovascular surgery, rapidly extended to applications in abdominal, gynecological, and oncological procedures, along with others.
Dr. Eleanor Matthews , a leader in minimally invasive techniques at a renowned teaching hospital, notes: “We realized that every incision we made, every muscle we cut, had a lasting impact on our patients. The drive to improve quality of life post-surgery has pushed us to continually refine our methods.”
This transition toward more patient-friendly procedures not only represents a technical achievement but also a profound change in the philosophy of surgical care.
The Rationale Behind the Procedures
Minimally Traumatic Surgery: Precision Enabled by Modern Tools
At the core of micro-invasive surgery is the principle of precision.
Practitioners harness an array of sophisticated instruments—from endoscopic systems and robotic devices to high-resolution microscopes—to navigate the human body through minute incisions.
Such devices offer superior magnification and lighting, thereby allowing accurate identification and intervention in the targeted zone with minimal tissue injury.
One of the most significant innovations has been the integration of robotic-assisted surgical systems.
These robotic-assisted platforms empower surgeons to achieve remarkable steadiness and exactness, eliminating natural hand tremors and transforming slight motions into precise, controlled maneuvers.
In surgeries like prostatectomies and cardiac operations, the attained precision brings about improved outcomes for patients.
Cardiothoracic Operations: Minimizing Cardiac Impact
Cardiothoracic surgery has also benefited significantly from micro-invasive methods.
Interventions such as valve repairs and coronary artery bypass grafting (CABG) have historically necessitated major incisions and broad muscle dissection.
Today, surgeons increasingly employ minimally invasive techniques that use small incisions and specialized instruments to access the heart and surrounding structures.
The integration of robotic-assisted systems into cardiothoracic procedures has further perfected these techniques.
In many cases, the robotic platform provides the precision required to perform delicate maneuvers on the beating heart, reducing the risk of complications and promoting faster recovery.
A study in the Annals of Thoracic Surgery demonstrated that patients who underwent minimally invasive valve repairs enjoyed lower rates of postoperative atrial fibrillation and reduced hospital stays when contrasted with conventional surgery.
General and Gynecologic Surgery: Enhancing Patient Outcomes.
Within general and gynecologic practices, minimally invasive methods have transformed interventions like gallbladder removals, hernia repairs, and hysterectomies.
Shifting to smaller incisions and prioritizing muscle preservation both reduces noticeable scarring and minimizes postoperative pain along with the risk of complications.
For instance, the laparoscopic removal of the gallbladder (cholecystectomy) via small incisions has become the norm in many areas.
Patients experience faster recuperation and can promptly resume their regular activities have a peek at these guys after surgery.
For gynecologic surgery, muscle-sparing strategies have been essential in achieving better outcomes for women facing complex operations like myomectomies or pelvic floor repairs.
An analysis published in a prominent medical journal observed that minimally invasive gynecologic procedures yield reduced infection rates and blood loss, plus enhanced cosmetic results.
These improvements serve to boost patient satisfaction as well as to yield better overall health outcomes.
Assessing the Pros and Cons.
Benefits Reaching Beyond Surgery.
The benefits of these micro-invasive and muscle-preserving techniques surpass the technical aspects of surgical procedures.
For patients, the benefits are tangible and life-changing.
Lower pain levels, decreased scarring, and quicker recovery periods directly contribute to a higher quality of life.
In many cases, patients can return to work and resume daily activities within days rather than weeks, a critical factor in an increasingly fast-paced world.
From his explanation a broader healthcare perspective, these techniques help lower hospital costs by reducing the length of hospital stays and the need for postoperative care.
Moreover, a reduction in complications leads to fewer patient readmissions, a critical factor for both healthcare providers and insurers.
The psychological benefits should not be underestimated.
Knowing that the surgery involves minimal bodily disruption provides significant reassurance and cuts down preoperative anxiety.
This factor is vital for patients scheduled for major surgeries, as a calm, optimistic outlook can enhance overall recovery and outcomes.
Challenges and Limitations: A Realistic Perspective.
Despite their many benefits, these minimally invasive and muscle-sparing techniques have limitations and challenges.
One notable challenge is the rigorous learning curve required for mastering these advanced methods.
Surgeons must undergo rigorous training and gain substantial experience before they can perform these procedures with the same level of proficiency as traditional surgeries.
The considerable initial investment in high-tech equipment and specialized training can be prohibitive, particularly in settings with limited resources.
Moreover, not all patients are ideal candidates for these approaches.
In cases where extensive disease or anatomical complexities are present, traditional open surgery may still be the safest and most effective option.
It is critical for surgeons to thoroughly assess every scenario, weighing the benefits of these methods against the individual patient’s requirements.
In addition, technical issues play a significant role.
Even with cutting-edge technology, limitations in the operative field or sudden complications may necessitate converting to a traditional open approach.
While uncommon, these cases highlight why it is essential to have a versatile and adaptive surgical team.
Clinician Insights and Patient Reflections
Voices from the Frontline
Dr. Michael Andersen, a renowned surgeon with over 25 years of experience in minimally invasive procedures, emphasizes the importance of individualized care
“Every patient is different, and while micro-invasive and muscle-sparing strategies yield substantial benefits, the primary aim is to modify the approach to suit the patient’s unique health status and overall condition,” he explains.
His insights underscore a fundamental tenet of modern medicine: technology must serve the patient, not dictate the treatment plan.
Similarly, patients who have undergone these procedures often speak of the transformative impact on their lives.
Maria Lopez, aged 54, who recently underwent a muscle-sparing breast reconstruction, details her experience candidly.
“I was ready for a drawn-out, painful recovery; however, I was up and active within days, feeling as though I had been reborn,” she remarks.
Such testimonials, while anecdotal, are supported by robust clinical data that points to improved outcomes with these techniques.
Establishing an Enduring Surgical Ecosystem.
The growing popularity of micro-invasive and muscle-sparing methods is fostering a broader cultural shift in healthcare.
Surgeons, hospitals, and training programs are increasingly collaborating to share best practices, develop standardized protocols, and invest in ongoing research.
Symposiums and conferences dedicated to minimally invasive methods are now routine in the medical arena, enabling experts to discuss innovations, hurdles, and future trends.
This collaborative approach is essential for addressing the challenges associated with these advanced techniques.
By pooling expertise and resources, the medical community is better positioned to refine surgical methods, reduce complications, and ensure that the benefits of these techniques are accessible to a wider population.
The Future of Surgery: Trends and Innovations.
Embracing Artificial Intelligence and Robotics.
Although today's micro-invasive and muscle-preserving methods have significantly influenced surgical practice, future innovations promise even more revolutionary transformations.
The integration of artificial intelligence (AI) and machine learning into surgical systems is poised to further enhance precision and efficiency.
These advanced tools analyze extensive data instantaneously, granting surgeons predictive guidance that may boost decision-making during challenging procedures.
For example, AI-powered imaging systems are being developed to automatically highlight critical anatomical structures, reducing the risk of inadvertent injury.
Robotic platforms are advancing continuously, with next-generation systems delivering enhanced precision and haptic feedback so surgeons can physically sense the tissue during procedures—a feature that traditional laparoscopic instruments do not offer.
Expanding the Scope of Minimally Invasive Techniques.
Ongoing advances in tissue engineering and regenerative medicine are expected to converge with innovative surgical practices.
Scientists are exploring ways to not only minimize tissue damage but also promote faster, more natural healing.
This includes the use of bioengineered scaffolds that can support tissue regeneration and reduce scar formation after surgery.
Moreover, as imaging and sensor technology continue to improve, surgeons may be able to perform procedures that are even less invasive than those currently available.
Innovations such as nanorobots and miniature, implantable devices could one day allow for targeted therapy and diagnostics at a cellular level, ushering in a new era of truly personalized medicine.
A Global Vantage: Uniting the Variances in Surgical Treatment
Although revolutionary tech-driven approaches are transforming surgery in well-resourced areas, notable gaps in securing advanced surgical services persist internationally
Bridging this gap calls for unified efforts from governmental bodies, non-profit entities, and the worldwide healthcare sector
Instructional programs, tech-transfer initiatives, and cooperative research projects are vital to ensure that patients around the world enjoy the advancements in micro-invasive and muscle-sparing procedures
Worldwide collaborations are beginning to show promising results
Institutions in high-resource regions are working in tandem with hospitals in developing locales to provide training and support for minimally invasive surgical techniques
These collaborative endeavors yield better patient care and contribute to establishing a more just international healthcare model
Charting the Path Forward: Obstacles and Prospects
The advancement toward full-scale integration of minimally invasive and muscle-sparing techniques is accompanied by various obstacles
The financial outlay needed for advanced technological tools, together with the requirement for dedicated training, is significant
Yet, the long-term benefits, including enhanced patient results and significant cost savings in healthcare, imply that these challenges are surmountable
Decision-makers and health system leaders are progressively understanding that channeling resources into cutting-edge surgical technologies can produce remarkable returns
Shorter periods of hospitalization, fewer clinical complications, and a swift return to work enhance patients’ quality of life while reinforcing a more resilient and efficient health system
Consequently, both public authorities and private organizations are starting to invest additional resources in advancing and spreading these methods
Additionally, there is a transformative shift occurring within the surgical profession's culture
The stress on ongoing learning, synergetic collaboration among various disciplines, and evidence-anchored practices is creating an ambiance where innovation is both welcomed and requisite.
The transformation in cultural ethos is set to foster the rapid integration of inventive methods and emerging technologies, ultimately conferring widespread benefits to patients.
Closing Remarks: A Transformative Move Toward Patient-Oriented Care.
The progression of micro-invasive and muscle-sparing surgical practices stands as a landmark change in how care is provided.
These procedures have redefined what is achievable in the operating theater through a commitment to accuracy, tissue conservation, and enhanced patient results.
From the formative stages of laparoscopic surgery to today’s blend of robotics and AI, the pathway has been paved with constant innovation and a resolute drive for excellence.
For patients, the promise is unmistakable: reduced pain, accelerated recovery, and a noticeably improved quality of life.
For healthcare providers, the task is to become skilled in these methods, invest in revolutionary technologies, and foster a continuous improvement culture.
With persistent progress in both research and technology, the scope for additional innovations in these surgical approaches is considerable.
The future of surgery envisions a patient-centric model where the well-being of the individual is paramount and surgical tools are designed to augment, not undermine, the body’s inherent resilience.
Peering into tomorrow, the combination of state-of-the-art imaging, robotics, and regenerative therapies is anticipated to unlock novel frontiers in patient-centered care.
The ongoing refinement of surgical methods is clear evidence of the healthcare sector’s promise to innovate, maintain high safety standards, and achieve improved patient results.
In a world where patient-specific care is paramount, micro-invasive and muscle-sparing surgical methods represent more than innovation—they offer a promise of a future where care is less invasive and recovery is enhanced.
As our journey advances, every innovation brings us closer to a reality where surgery is not a precursor to pain and extended recovery but a stepping stone toward renewed health and vitality.
References and Further Reading.
Clinical Studies and Reviews: Numerous scholarly articles in journals such as the Journal of Minimally Invasive Surgery, Annals of Thoracic Surgery, and the Journal of Surgical Education deliver extensive data on the benefits and outcomes of these surgical techniques.
Expert Interviews: Perspectives from expert surgeons, including Dr. Eleanor Matthews, Dr. Luis Hernandez, and Dr. Michael Andersen, provide detailed commentary on the practical challenges and advantages of micro-invasive and muscle-sparing procedures.
Technological Innovations: The latest developments in robotic-assisted surgery and augmented reality are well chronicled in contemporary medical publications and discussed at international surgical meetings.
Micro-invasive and muscle-preserving techniques have launched a transformative era in patient-focused care. Through an emphasis on accuracy, reduced operative trauma, and muscle conservation, these methods improve both clinical results and patient satisfaction.
As the pace of technological evolution quickens and global acceptance of these methods increases, the future of surgery is set to provide even more transformative benefits for patients.
Within this dynamic field, an unwavering commitment to continuous progress is the genuine measure of success—a pledge that will reimagine surgical care for generations.
 Danny Tamberelli Then & Now!
Danny Tamberelli Then & Now! Joseph Mazzello Then & Now!
Joseph Mazzello Then & Now! Michael Jordan Then & Now!
Michael Jordan Then & Now!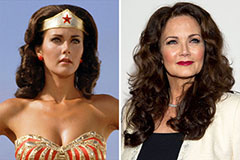 Lynda Carter Then & Now!
Lynda Carter Then & Now! Dawn Wells Then & Now!
Dawn Wells Then & Now!